TW: This article discusses assisted death and suicide
The Swiss company Sarco developed a ‘suicide pod’ in December 2021 that fills with nitrogen so a person loses consciousness and dies within 10 minutes. While the pod creates a convenient method of death, many question the ethics behind this system, leaving the world to wonder about the future of assisted death.
Assisted death means taking one’s life with the help of a physician to end severe terminal illness. In the U.S, ten states and Washington D.C. have legalized assisted death, including California. However, other countries, such as Switzerland have a much more lenient policy. As the world approaches epic heights in COVID deaths, countries begin to reevaluate their approach to assisted death, including California.
First Hand Experience
Unlike Switzerland’s progressive take on assisted death, California follows a rigid legal system that many have found difficult to work with. After Palo Alto resident Erica Rui underwent the loss of both parents this past year, this event greatly influenced her perspective on assisted death.
“After taking care of my father and mother, and then seeing how they suffered toward the end, I just thought it would be [easier] if they could go without further pain and suffering … instead of giving them mass amounts of painkillers to stop the pain and prolong their life,” Rui said.
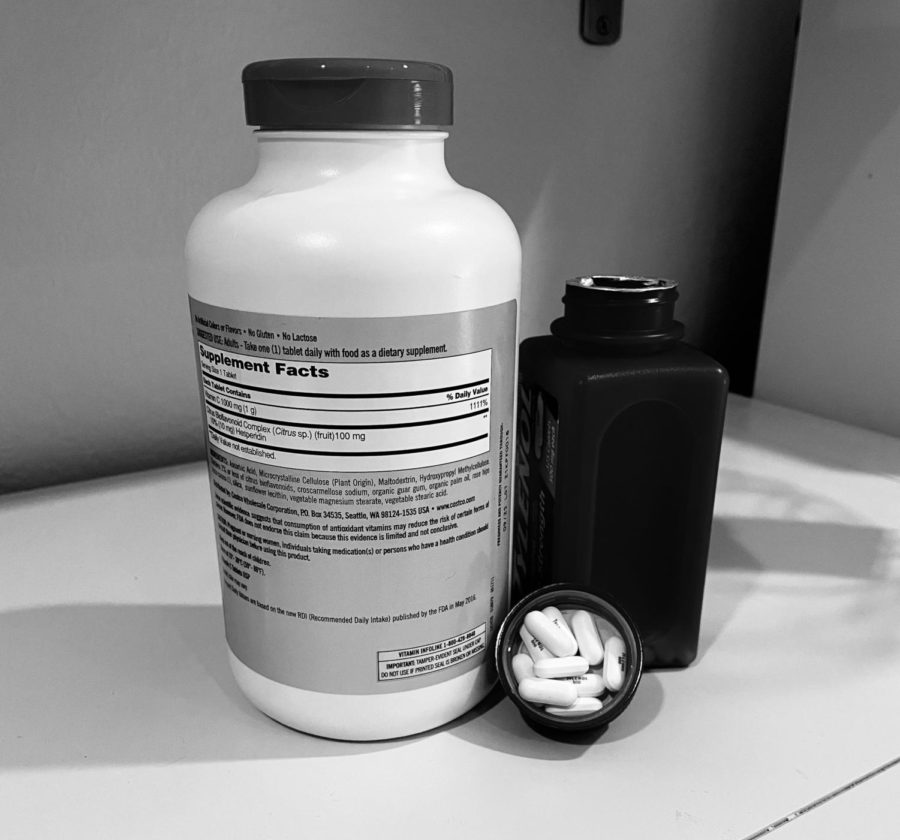
However, the process of qualifying for assisted death in the state of California requires many steps. Currently, the patient must have a diagnosis of a terminal illness with a life expectancy of about six months, confirmed by two physicians. Two oral requests must be made by the patient with, as of October 2021, a two-day waiting period between requests.
“Then, once you’ve made these requests … you would be prescribed the drug,” a Woodside parent and local physician who wished to remain anonymous said. “You have to be mentally competent to administer it yourself, … no one can give it to you … The thought is to protect people from having family members or friends try to help them. The way the drug works is that it works on the nervous system to turn it off so you stop breathing.”
In the case of Rui’s parents, who both died in their 90s, with her father passing away about a month ago due to continuous health problems, assisted death wasn’t an option. During their final months, Rui watched as her parents were unable to leave the house or do the activities they loved. For Rui, this was emotionally straining and put a burden on the family.
“My father always said ‘Oh, I’m going to go, I’m going to go,’ and yet it’s very hard for us as children [to watch],” Rui said. “This is my parents and I don’t want to see you guys leave. Yet all he can do is just lie in bed and cannot do anything and everyone else had to help. It’s just not one family member, many family members have to come to help.”
Watching loved ones suffer is both a mentally and financially burdensome task put on family members when those who are terminally ill have very little control of their life. For Rui’s father, that meant 24/7 support and help.
“What is the quality of life?” Rui said. “There’s absolutely no quality of life. You’re basically counting on meditation to prolong your life. But then you cannot go anywhere, people need to be around just to make sure you take the medicine, to take the food, and then virtually there’s nothing to do. Then why do you need to go on when you cannot go out and enjoy your life?”
For many patients, the stage of no recovery is when many qualify for assisted death. At this point, there is very little quality of life, such as in the case of Redwood City resident Benjamin Manarello’s friend.
“I recently had a friend whose dad died at age 52,” Manarello said. “He died because he had heart complications, an aneurysm, and a stroke all at the same time. He was seizing and in the hospital, basically a vegetable … [while] on a respirator, and it was better off letting him go at that point.”
Due to California’s recent change in assisted death laws, nursing homes underwent different procedures when dealing with assisted death.
“I think the new law in California makes facilities, like hospice facilities where a lot of the patients may consider something like this, have to post their policies on ending life options [to patients],” Woodside parent and local physician said.
However, with the extensive precautions the nursing home put in place due to COVID, family members such as Rui were unable to be by her mother’s side in her last moments. This put stress on both Rui’s family and mother.
“When my mother was in the nursing home, that was very hard because someone else is helping her instead of a family member,” Rui said. “Then when COVID came, that made everything harder as they had to take COVID precautions, versus having a family member there all the time. … This way also sort of shortens their life because they have no loved ones.”
For many older people, the primary patients of assisted death, COVID became a leading cause of death in the past year. While many relied on respirators to keep them alive, the question of whether assisted death could have relieved the suffering lingers.
“With COVID it’s difficult to say because it’s still very new,” Rui said. “I think with COVID there’s still a lot of hope of getting well. Versus the long-term illness, then you know you’re going to go. I think with COVID [assisted death is] a very last resort. I think the [circumstances for assisted death] are a little different.”
Should Assisted Death be Legalized?
Despite assisted death not often used with COVID patients as it usually doesn’t fall within the qualifications as per the California law, this current system provides more for patients who prefer this route in life than other states. Many people question whether assisted death should be legalized in more places.
“I think it should be legalized because some people have legitimate reasons for wanting to die,” Woodside freshman Natalie Gerola said. “Prolonging someone’s life isn’t always the best situation because [they could be] miserable [due to] health reasons that are severe. [If] they can’t live on their own and they don’t want to live on their own then it’s not really fair to them to keep them living.”
For physicians, however, the idea of assisted death contradicts that of their normal practice. As the Hippocratic oath, the text new physicians swear by, states, ‘Do no harm.’ Yet assisted death contradicts this ideology.

“We try to keep people healthy and we want everyone to live a long life, so the thought of helping someone end their life seems contrary to being a physician,” Woodside parent and local physician said. “That being said, some physicians would argue that helping people end their suffering when they have a terminal illness is helping their patients.”
Currently, many places in the U.S. hold strict policies against assisted death due to religious reasons. Many allow physicians to opt out of helping patients with assisted death.
“In the U.S. there are a lot of health care systems that are religious or they are affiliated with certain religions so they have certain policies that they won’t participate in this type of thing,” Woodside parent and local physician said.
Whether it be assisted or natural, people hope that individuals find peace in their death.
“There’s a much better way if we’re going to die, we’re gonna die. It will be best to go the way we want to, without any deep suffering,” Rui said.